Murrell Bradley – Hummelstown, PA
Died: January 6th, 2022
Hershey Medical Center – Hershey, PA
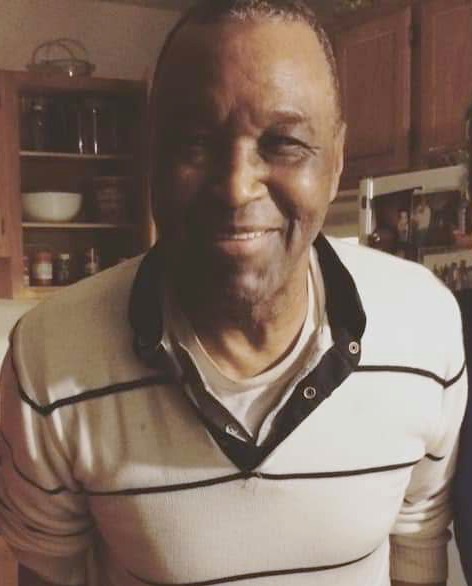


Murrell’s story is being told today by his daughter, Deanna Slamans. Murrell served in the Pennsylvania Army National Guard as a military police officer and was an employee at the former Bethlehem Steel Corporation., as a crane operator. He was brilliant and very talented. He played the flute and was gifted in drawing and also loved playing chess. Murrell had a beautiful singing voice and was a member of United Baptist Church, where he sang on the choir. When he was younger, he sang in a quartet with his brothers and their father. Murrell was a thinker. He liked to read, watch the news and talk about current events and politics. He enjoyed being with his family and loved being a grandfather.
My father’s name is Murrell Bradley. He entered the Hershey Medical Center, in Hershey, PA around 8:30 PM on December 22. The reason we called the ambulance is because upon visiting him he was confused, short of breath and very thirsty. He had urinated on himself because he was too weak to use the restroom. He has never done that before. I had never seen him so weak. He was trembling. When the EMT arrived his blood oxygen level was 88%.
Upon arriving at the ER they tested him for COVID. They also said his kidneys were malfunctioning and his pulse was very rapid, in the 170s. They hydrated him and placed him on a low level of oxygen to saturate it while they waited for test results.
When the results ended up being COVID positive they admitted him and continued to treat his kidneys and heart rate. He was not in respiratory distress. I have the medical records that state that as a fact.
Once admitted I was told I could see him. It was Christmas Eve. My twin sister was also in Holy Spirit Hospital in Camp Hill from a hit and run accident and she was on life support. She had two brain bleeds and a fractured skull. So, I chose to visit her because I thought she would die that day.
I spoke to my father on Christmas day and he sounded good. He called me by my nickname “Little Bit” and I wished him a Merry Christmas. I asked him if he knew he had COVID and he said they had not told him that.
On December 26, his kidney functions returned to normal and his heart rate in the low 90s which is typical for the elderly. He was still on the oxygen and they said it was now at 94% with the hi-flo vent nasal cannula.
On December 27, I received a call from his attending physician stating it was urgent and that I needed to decide to intubate him. Immediately I went to the hospital (it is 10 min.) from my home. When I arrived, I was told I could not go and see him. I argued that there were visiting hours over the Christmas holiday. They said the rules had changed.
I called the attending physician back, Dr. Aktbar (sp?) back and asked if she could prescribe to my father Regeneron. I was told he was not a candidate because he had the Omicron variant and that one was resistant to the antibody treatment. But when I asked if she had performed a genome sequencing for that variant on my father, she said they had not. She just assumed he had that variant.
That is when I got upset. I knew then that she had lied to me and could have been lying to me about all sorts of things. I asked if she could consider treating him with IVM before the intubation. She said it is not their protocol and it is not effective. I requested HCQ. She gave me the same reason. The EUA did not permit that. She stated that he was unvaccinated and that their protocol was intubation for the unvaccinated.
I asked her what the likelihood of him recovering on a ventilator was. She said it usually doesn’t end up good. So I told her that her treatment doesn’t work and that she needed to find other acceptable treatment for my father. She did not respond.
I then asked her if they were at least giving him Vitamin D, Zinc, and NAC. She said no. I asked why not, because he is vitamin D deficient. She did not answer me. I left the hospital in a puddle of tears. I came home and told my children and husband that Grandpa was going to die in the hospital. That day he was placed in the COVID ICU.
I had hydroxychloroquine at home and IVM, but I was not permitted to visit him. Our family thought of taking him out of the hospital, but it was the holidays, we were unsure of the availability of a visiting nurse or anyone at that time of the year.
On December 28, I was introduced to Dr. Mole in the Medical ICU. They continued to treat my father with the nasal cannula at my request. That evening they began to place my father on a BIPAP facemask at night (not sure why at night), to help keep his oxygen levels up. They began treating him with dexamethasone. They had refused remdesivir due to his liver screening results.
In the meantime, I am continuing to visit my twin sister who is unconscious and has no idea our father is fighting for his life.
On December 29, I was told by Dr. Mole that my father was stable and improving! They continued to cannula but were giving him dexamethasone and an antibiotic for what they said is covid pneumonia. But I had been told previously his lung scans were clear, and have the medical records to prove it.
On December 30 and December 31, I spent a lot of time on the phone with Dr. Baric and Dr. Ruben who kept insisting my father needed to be intubated. He was pulling the bipap machine off because he was aggravated with it on. I told them to figure out a way for him to keep it on. I also asked if they had been giving him his haldol. He takes it for schizophrenia. They stated they had not been. It calms him some.
I requested a meeting with the hospital social worker. She told me the hospital had agreed to a meeting with me. I continued to suggest other therapies. Instead, they explained his oxygen levels were poor, and they let me see him, FINALLY! He was lucid, and we joked some. He said he missed us, and our puppy, River, laughing. He was sedated but just had the BIPAP machine on.
On January 1, they intubated him because he kept pulling his mask off. They began the rotation of flipping him on his stomach (prone) for 16 hours and on his back (supine) for 8 hours. This was to get rid of the CO2 build up in his lungs. They continued him on the ventilator for 5 days.
On January 6 around 6:30 AM I was called and told he was losing oxygenation quickly. His heart stopped in the middle of the night when the nurse turned his head. At 7:00am I went with my children to say goodbye to my father. He was pronounced dead at 7:40AM.